Signs And Symptoms Of High Calcium Levels – Is a free educational content provider. If you want to support our (caffeinated and sleep-deprived) editors, fill out the information below to let us know who uses the site. To prevent this pop-up from appearing frequently, we use cookies. Continue to use the site if you are happy with it.
The following module has been designed to complement the study of medical students in the clinic. Please take the time to read each module by clicking on the headings below. Information on how to diagnose and manage hypercalcemia.
Signs And Symptoms Of High Calcium Levels

Hypercalcemia of malignancy is common in advanced stage cancer affecting more than 40% of patients (1). Calcium levels require tight regulation and small deviations from normal can cause significant morbidity.
Vitamin D And Your Health: Breaking Old Rules, Raising New Hopes
The vast majority of the body’s calcium is stored in the bones and very little is in the blood, with about 65% of blood calcium bound to albumin, which is unavailable for use (1). Low serum calcium levels stimulate the parathyroid glands to release parathyroid hormone, which increases calcium levels in 3 ways: renal tubular reabsorption, vitamin D activation, and mobilization from bone (1). Vitamin D increases calcium absorption from the GI tract and decreases renal excretion (1). On the other side of regulation, calcitonin is a hormone released by parafollicular/C cells in the thyroid gland that is involved in lowering serum calcium by inhibiting renal reabsorption and mobilization of calcium from bone (1).
There are several mechanisms of hypercalcemia of malignancy, including humoral hypercalcemia mediated by increased parathyroid hormone-related peptide (PTHrP), local osteolytic hypercalcemia due to bone breakdown, excessive extrarenal activation of activated vitamin D that promotes calcium reabsorption/retention, and excessive ectopic or primary secretion of PTH ( 2). The PTHrP mechanism is the most common (80%) and it is the peptide’s structural similarity to endogenous PTH that drives increased tubular renal calcium absorption, decreased renal excretion, and stimulates osteoblasts to produce RANKL. Local osteolytic hypercalcemia accounts for approximately 20% of bone tissue hypercalcemia and is thought to be caused by excessive osteoclast activation and bone resorption due to tumor cytokine secretion (2).
A classic mnemonic for the symptoms of hypercalcemia is “rocks, bones, abdominal groans, and psychic undertones.” In addition, there are characteristic features of the cardiovascular system of hypercalcemia.
When hypercalcemia is suspected, the first step in the investigation is to measure serum calcium and serum albumin (if serum albumin is abnormal, the measured calcium should be adjusted). Once PTH, PTHrP, and vitamin D levels are confirmed, they will help characterize the cause of the hypercalcemia.
Hypercalcemia And Hypocalcemia Notes: Diagrams & Illustrations
The first step in treatment is fluid resuscitation with IV normal saline. Patients with hypercalcemia due to bone metastases are usually dehydrated due to nausea, vomiting, loss of appetite, and hypercalcemia-induced nephrogenic diabetes insipidus. All of these factors contribute to volume depletion and promote a cycle of further elevation of serum calcium (1). In addition to fluids, there are several medications used to lower serum calcium. Exogenous calcitonin has a rapid onset of action and is a good initial therapeutic option when transitioning to longer-term therapies (1). It is effective within 4 hours, but tachyphylaxis often develops around 48 hours and should therefore only be used in the transition period to start maintenance therapy (2). Bisphosphonates (eg, zoledronic acid and pamidronate) are used as longer-term therapy, but their calcium-lowering effect lasts 2–4 days (1). In patients with high PTHrP levels, bisphosphonates may be less effective and other treatment options such as denosumab may be another treatment of choice, although this use is off-label (1). Hemodialysis should be considered in patients who cannot be safely rehydrated due to cardiovascular disease.
Note: This case can be filled on an iPad. To do this, download the (free) Articulate mobile player for iPad by clicking here. Calcium is important to humans because it helps with muscle contraction, nerve conduction, blood clotting, and the release of enzymes and hormones. There are several regulatory mechanisms that keep blood calcium in the normal range, disruption of which can cause low or high blood calcium levels.
C. In case of primary hyperparathyroidism, a special scan of the parathyroid glands is necessary to localize the adenoma along with an assessment of bone mineral density

Surgical treatment: The surgical procedure will involve removing the affected gland or removing more than three glands if all glands are overactive.
Oncologic Emergencies With Dr. Aditi Singh
Once the cause of hypercalcemia is identified, treatment should be directed at that well. If the reason is an overdose of vitamin D, it’s easy, we have to stop the vitamin. More difficult if it is due to malignancy, usually in most cases high calcium is a late sign and we can only offer a palliative acr.
A transient, mildly low calcium level is common after surgery. In some cases, low calcium can remain permanent when you need calcium and vitamin D treatment.
Hungry bone syndrome may develop if an overactive parathyroid has persisted for some time prior to surgery. This causes a rapid influx of calcium into the bones, causing prolonged hypocalcemia.
Whatever treatment or surgery is done, we need lifelong follow-up at regular intervals, sometimes maybe once a year. This high yield note provides an overview of the essential elements of hypercalcemia and hypocalcemia. All notes are clearly laid out and feature striking images, tables and diagrams to help visual learners understand complex topics quickly and efficiently. For more information on hypercalcemia and hypocalcemia, see:
Hyperparathyroidism: Elevated Pth, Symptoms, And Surgery
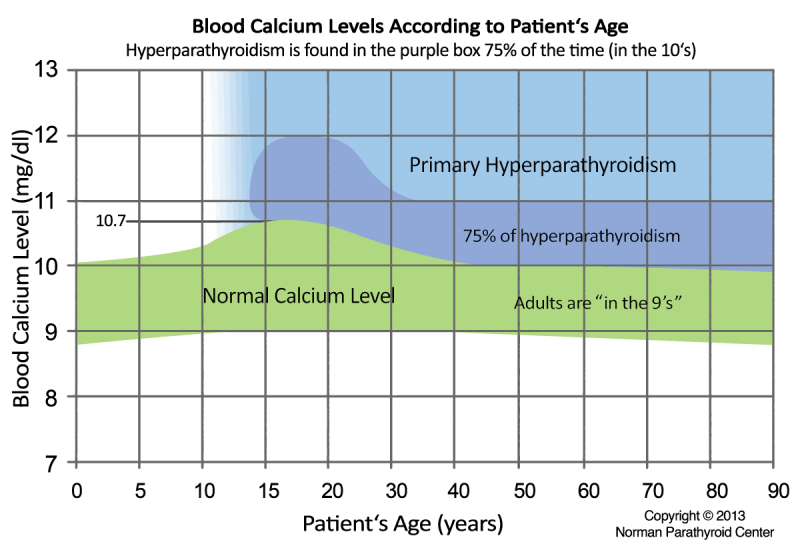
NOTES NOTES HYPERCALCEMIA AND HYPOCALCEMIA IN GENERAL, WHAT ARE THEY? PATHOLOGY AND CAUSES ▪ Blood calcium concentration falling outside the normal reference range ▪ Hypocalcemia: 10.5 mg/dL SIGNS AND SYMPTOMS ▪ Changes that are mild or slow-onset, usually asymptomatic ▪ Hypercalcemia → less excitable neurons and related symptoms across multiple systems ▪ Hypocalcemia → more excitable neurons and related symptoms across multiple systems DIAGNOSIS LAB RESULTS ▪ Blood calcium levels ▪ Determination of underlying cause (blood tests for levels) ▫ Parathyroid hormone, vitamin D, albumin, phosphorus , magnesium ADDITIONAL DIAGNOSIS ECG ▪ Identify associated organ dysfunction TREATMENT DRUGS Hypercalcemia ▪ Lower blood calcium ▫ Rehydrate, loop diuretics, glucocorticoids, bisphosphonates or calcitonin, dialysis hypocalcemia ▪ Increase calcium ▫ Calcium gluconate supplement▫44
Chapter 111 Hypercalcemia and Hypocalcemia HYPERCALCEMIA osms.it/hypercalcemia PATHOLOGY AND CAUSES ▪ High blood calcium (> 10.5 mg/dL) ▪ True hypercalcemia caused by an increase in free ionized calcium (not bound to proteins, which is 40-45% of total calcium ) CAUSES Excessive bone resorption ▪ Hyperparathyroidism ▫ Most common cause ▫ Increased osteoclastic bone resorption ▫ Overactive parathyroid glands → releases more parathyroid hormone → stimulates osteoclasts → osteoclasts break down bone → release calcium into blood ▪ Thyrotoxicosis ▫ hormone-mediated increase in bone resorption ▫ Can secrete protein related with parathyroid hormone (PTHrP) ▫ May cause osteoblast cell death ▫ May also cause excessive stimulation of osteoclasts → lytic bone lesions ▫ May directly attack bone ▪ Less common causes ▫ Immobilization, Paget’s disease of bone, anti-estrogen therapy, hypervitaminosis A (retinoic acid → dose-dependent increase in bone resorption) ▫ Thiazide diuretics (increase calcium reabsorption in the distal tubule of the kidney) ▫ Lithium (increase calcium reabsorption from the loop of Henle, also interferes with normal hypercalcemic feedback to the parathyroid gland) ▫ Calcium carbonate supplementation ▪ Milk-alkali syndrome ▫ Extra calcium from diet, bases contained in antacids) ▫ Hypercalcemia, metabolic alkalosis, renal insufficiency Insufficient excretion ▪ Adrenal insufficiency (e.g. Addisonian crisis) ▪ Adrenal failure (eg rhabdomyolysis) False hypercalcemia / pseudohypercalcemia ▪ Hyperalbuminemia → ↑ albumin → ↑ protein-bound calcium → ↑ total calcium ▫ Free ionized calcium concentrations remain the same (hormonal regulation) ▫ High total calcium, free ionized calcium normal ▫ Rare cause: dehydration COMPLICATIONS ▪ Calcium oxalate kidney stones (hypercalciuria, fluid loss) ▪ Osteoporosis (depletion of calcium stores in bones) ▪ Kidney failure ▪ Cardiac arrhythmia ▪ Confusion, dementia, coma Excessive absorption of calcium ▪ Excessive absorption of vitamin D ▫ Stimulates active intestinal absorption, bone resorption, and increased renal reabsorption ▪ Diet or excessive supplementation ▫ When intake exceeds 2 grams per day, passive transport can also lead to hypercalcemia ▪ Drugs 795
SIGNS AND SYMPTOMS ▪ Many individuals are asymptomatic ▪ Slow chronic onset, better tolerated ▪ Neurological ▫ Neurons less excitable ▫ Blurred vision, slow or absent reflexes ▫ Central nervous system: fatigue, anxiety, confusion, hallucinations, rigidity ▪ Cardiovascular ▫ Arrhythmias, shortened arrhythmias , bradycardia, hypertension. blood calcium levels > 10.5 mg/dL ▪ Calcium levels must be adjusted to albumin levels or free ionized calcium measured ▫ Albumin: may be ↑ in pseudohypercalcemia ▪ Parathormone: ↑ or ↓ ▪ PTH-related hypercalcemia: primary hyperparathyroidism and familial hyperparathyroidism ▪ Non-PTH-related hypercalcemia: primary malignancy, vitamin D intoxication, granulomatosis ▪ PTH-related peptide: may ↑ in certain malignancies 796 ▪ Vitamin D: may be ↑ intoxicated ▪ Phosphate: ↑ or ↓ depending on PTH (high renal insufficiency, hypoparathyroidism , low vitamin D deficiency) ▪ Magnesium: hypercalcemia can ↓ Mg levels OTHER DIAGNOSIS ECG ▪ Bradycardia

High levels of calcium, signs and symptoms of high sugar levels, signs and symptoms of high thyroid levels, signs and symptoms of high cortisol levels, signs and symptoms of high potassium levels, signs and symptoms of high glucose levels, signs and symptoms of high ammonia levels, symptoms of high calcium levels in blood, signs and symptoms of high tsh levels, signs of high calcium levels, symptoms of high calcium levels, signs and symptoms of low calcium levels