Mast Cell Disease Low White Blood Count – Open Access Policy Institutional Open Access Program Special Issues Guidelines Research Editorial Process and Publication Ethics Article Processing Fees Awards Testimonials
All articles published are immediately available worldwide under an open access license. No special permission is required to reuse all or part of an article published by , including figures and tables. For articles published under the Creative Commons CC BY open access license, any part of the article may be reused without permission, provided the original article is clearly cited. For more information, see https:///openaccess.
Mast Cell Disease Low White Blood Count

Distinctive papers represent cutting-edge research with significant potential for major impact in the field. A feature paper should be a substantial original article that incorporates several techniques or approaches, provides an outlook for future research directions, and describes possible research applications.
Photos That Show What Mast Cell Activation Disorder Looks Like
Distinctive papers are submitted by individual invitation or recommendation from scientific editors and must receive positive feedback from reviewers.
Editor’s Choice articles are based on recommendations from scientific journal editors from around the world. The editors select a small number of articles recently published in the journal that they believe will be of particular interest to readers or important in the relevant area of research. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
By Clayton Webster Jackson Clayton Webster Jackson Scilit Preprints Pattanaik Debendra Pattanaik Scilit Preprints.org Google Scholar View Publications 3 and Guha Krishnaswamy Guha Krishnaswamy Scilit Preprints.org Google Scholar View Publications 1, 4, *
Original submission received: September 16, 2021 / Revised: October 14, 2021 / Accepted: October 15, 2021 / Published: October 19, 2021
White Blood Cell Count And Major Adverse Cardiovascular Events After Percutaneous Coronary Intervention In The Contemporary Era
Mast cells are derived from hematopoietic stem cell precursors and are essential for the genesis and manifestations of the allergic response. Activation of these cells by allergens leads to degranulation and elaboration of inflammatory mediators, responsible for regulating the acute dramatic inflammatory response. Mast cells have also been implicated in various diseases such as malignancy, arthritis, coronary artery disease and osteoporosis. There has been a recent explosion in our understanding of mast cells and the associated clinical conditions that affect this cell type. Some mast cell disorders are associated with specific genetic mutations (such as the D816V gain-of-function mutation) with resultant clonal disease. Such disorders include cutaneous mastocytosis, systemic mastocytosis (SM), its variants (indolent/ISM, smoldering/SSM, aggressive systemic mastocytosis/ASM), and clonal (or monoclonal) disorders or mast cell activation syndromes (CMCAS/MMAS). In addition to clonal mast cell activation disorders/CMCAS (also known as monoclonal mast cell activation syndromes/MMAS), mast cell activation can also occur secondary to allergic, inflammatory, or paraneoplastic disease. Some disorders are idiopathic because their molecular pathogenesis and evolution are unclear. A genetic disorder known as hereditary alpha-tryptasemia (HαT) has also recently been described. This condition has been shown to be associated with increased severity of allergic and anaphylactic reactions and may variably interact with primary and secondary mast cell disease, resulting in complex combined disorders. The role of this review is to clarify the classification of mast cell disorders, point out the molecular aspects of mast cell signaling, elucidate the underlying genetic defects, and provide approaches to targeted therapies that may benefit such patients.
Since the discovery of mast cells (MCs) in the nineteenth century, our knowledge of these fascinating and multifunctional cells has grown exponentially [ 1 , 2 , 3 , 4 , 5 ]. During the last few decades, diseases related to mast cell function and biology have been described. Mast cells orchestrate typical allergic conditions where activation of these cells by allergens (such as food, Hymenoptera venom, latex, antibiotics and pollen) leads to degranulation and elaboration of inflammatory mediators, responsible for regulating the acute dramatic inflammatory response observed [6, 7, 8]. Mast cells modulate angiogenesis, inflammation and tissue repair, innate and adaptive immune responses, immune tolerance, and host defense [ 9 ]. As a consequence, mast cells have also been implicated in a wide variety of disorders such as Crohn’s disease, malignancy, autoimmunity (including Guillain-Barre syndrome, Sjogren’s syndrome, vasculitis, and inflammatory arthritis), multiple sclerosis, coronary artery disease, arterial aneurysms, and osteoporosis [1, 3, 9, 10, 11]. Expansion of mast cell populations also occurs in chronic infections (parasitic infestations, tuberculosis, and syphilis), melanomas, chronic kidney and liver diseases, and scleroderma [12].
Some mast cell disorders are associated with specific genetic mutations resulting in clonal disease (Table 1). Such disorders include cutaneous mastocytosis, systemic mastocytosis (SM), its variants (indolent/ISM, smoldering/SSM, aggressive/ASM) and some forms of recently described mast cell activation disorders or syndromes (MCAD or MCAS) [13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24]. The latter include clonal mast cell activation disorders / CMCAS (also known as monoclonal mast cell activation syndromes / MMAS), mast cell activation secondary to allergic, inflammatory or paraneoplastic disease and idiopathic disorders [16, 22, 25, 26, 27, 28]. These conditions have been better understood by the medical community in the last few decades due to advances in cell biology and molecular techniques, leading to improved attempts at classification and prognosis [ 15 , 29 , 30 , 31 ]. The most commonly observed gain-of-function mutation (KIT D816V) is a somatic A to T missense mutation and involves the substitution of aspartic acid (D) with valine (V) at amino acid 816 in exon 17 of the KIT gene (a proto-oncogene also known as c- KIT), which encodes the KIT protein (CD117 or stem cell factor receptor/SCFR), a receptor tyrosine kinase. This transmembrane receptor binds to stem cell factor (SCF), initiating a signaling cascade in mast cells, regulating their growth, development, migration and proliferation. In some situations, clonality is also determined by aberrant cellular expression of CD25 (IL-2 receptor alpha chain) or CD2 (lymphocyte function antigen-2 or LFA-2) on neoplastic mast cells. In addition to the above cluster of conditions, hereditary alpha-tryptasemia (HαT), described recently, has been shown to be associated with increased severity of allergic and anaphylactic reactions.

This article attempts a translational clinical-molecular review of a rapidly evolving but fragmented literature, which makes it confusing. We’ve combined information on mastocytosis, mast cell sarcoma, mast cell activation disorders, hereditary alpha-tryptasemia, and idiopathic allergic/mast cell disease in one place, with updated criteria for diagnosis and management overview. The role of this review, therefore, is to clarify the classification of mast cell disorders, point out molecular aspects of development, and provide evidence for broad targeted therapies that may benefit such patients. This is not meant to be an exhaustive review of mast cell biology or mast cell-related pathology.
Heavy Metals, Mast Cell Activation, And Histamine Intolerance
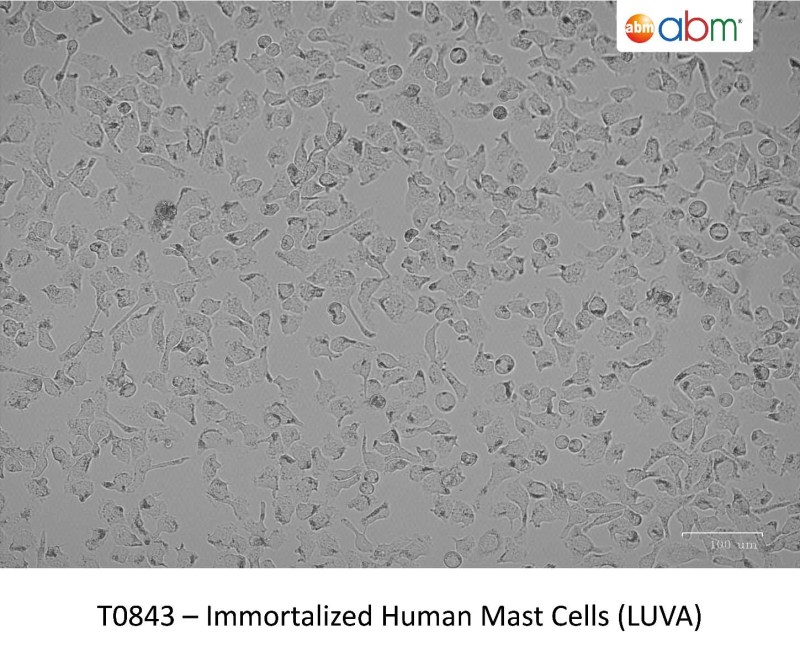
Human mast cells, first described by Paul Ehrlich, are multifunctional immune cells of the myeloid lineage, intimately involved in allergic reactions [ 1 , 2 , 3 , 5 , 32 , 33 ]. Mast cells originate from CD34
Multipotent, hematopoietic progenitors [4, 5]. They migrate to peripheral tissues and undergo differentiation and maturation under the influence of growth factors, including stem cell factor (SCF), where interactions occur with other cell types, including eosinophils and T cells [2, 3, 4, 5, 34, 35]. SCF is a mast cell chemoattractant that also affects mast cell proliferation, differentiation, maturation, adhesion, and survival. SCF binds to its receptor, KIT, a transmembrane receptor and signal-coupled tyrosine kinase [ 36 , 37 , 38 , 39 ]. Somatic mutations in c-KIT encoding the KIT receptor (the most common of which is the D816V mutation) are associated with the development of systemic mastocytosis, a clonal hematological disorder [40].
Under the influence of local tissue-derived maturation factors, mast cell differentiation results in the development of well-recognized phenotypes: mucosal mast cells (mainly tryptase-expressing or MCT cells, located predominantly in the mucosa) and alveoli and connective tissue mast cells (expressing tryptase, chymase and carboxypeptidase A3 or MC-TC, located in submucosal and connective tissue sites such as the skin) [2, 3, 4, 5]. Atyakshin et al demonstrated the colocalization of tryptase and chymase in the same mast cell granules using sophisticated immunohistochemical techniques [41]. In Th2-mediated diseases, such as atopic asthma and nasal polyposis, intraepithelial MC-T cells may undergo structural changes. The unique co-expression of tryptase and carboxypeptidase A3 has been demonstrated by MC-T cells under these circumstances [ 42 ]. Dvorak described the finer aspects of mast cell ultrastructure, such as the expression of scroll-containing granules, crystal-containing granules, particle-containing granules, particle-filled granules, or mixed types observed under electron microscopy [43].
Mast cells undergo maturation in target tissues under the influence of interleukin (IL)-3, IL-4, IL-9, IL-33, CXCL2, SCF, nerve growth factor (NGF) and transforming growth factor beta (TGF- β1 ) [4, 5]. Autocrine expression of SCF by mast cells is hypothesized to represent mast cells regulating their own growth and survival [5].
Pdf) White Blood Cell Count Profiles In Multiple Sclerosis During Attacks Before The Initiation Of Acute And Chronic Treatments
Mast cell activation can occur following many triggers and through a plethora of cell surface receptors, including receptors for IgE, IgG, complement, cytokines, growth factors, stem cell factor, and neuropeptides (beyond the scope of this review) [4, 11, 33]. Prototypical IgE-mediated activation (Figure 1) occurs when allergen-specific IgE binds to a multivalent allergen and interacts with the high